
- #Timely filing for medicare home health ceertification manual#
- #Timely filing for medicare home health ceertification full#
- #Timely filing for medicare home health ceertification license#
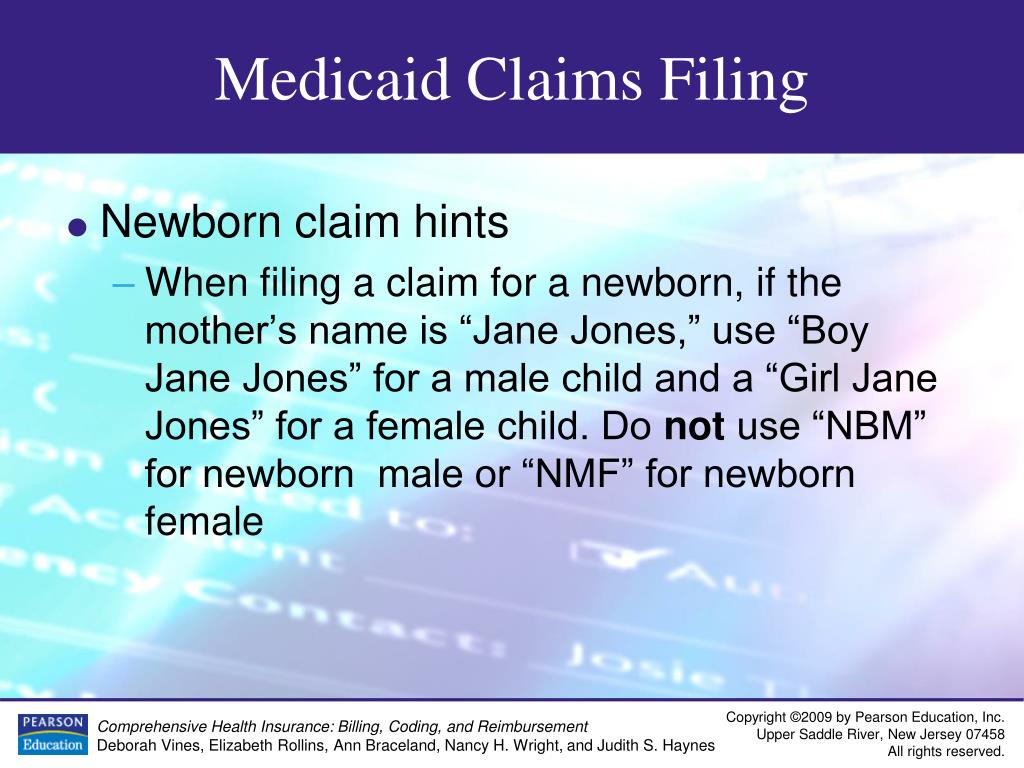
All claims must be submitted to Idaho Medicaid within twelve months (365 days) from the date of service.
#Timely filing for medicare home health ceertification license#
The requested effective date must be noted and must be covered by any applicable license or certification submitted with the application. Typically approved exceptions include emergency services or covered specialist services that otherwise would be available to a Medicaid Participant. The effective date of an applicant's enrollment as an Idaho Medicaid provider is deemed to be the date the completed and acceptable application is received by the Department of Health and Welfare or Gainwell.Īny exceptions to this policy must be requested in writing, providing justification as to why the applicant's effective date should be different. Women's Cancer Screening (Women's Health Check).Alzheimer’s Disease and Related Dementias.Per and Polyfluoroalkyl Substances (PFAS).Women's Health, Fit & Fall, Quit Smoking.Medicaid for Elderly or Disabled Adults.Medicaid for Children with Disabilities.Supplemental Nutrition Assistance Program (SNAP).Temporary Assistance for Families in Idaho (TAFI).Aid to the Aged, Blind, and Disabled Cash Assistance (AABD).Child and Family Services and Foster Care.Death, Stillbirth, and Miscarriage Records.
#Timely filing for medicare home health ceertification manual#
Medicare Benefit Policy Manual - Chapter 7: Home Health Services.Providers are encouraged to submit their prior authorization requests to ensure timely clinical review and reimbursement. Other supportive clinical documentation.Retrospective Home Health Services Request Form.Fax should include the following documents: Failure to do so risks denial of some or all services (including those already delivered). Fax the request form to HPSM within seven days from start of care.
#Timely filing for medicare home health ceertification full#
This should alleviate duplicative start of care visits. Please coordinate and confirm with the referral source that orders have been received and the start of care visit will be scheduled within a reasonable time after hospital discharge.

We ask that providers submit requests according to the clinical need/clinical presentation of the member based on assessment. Learn more about prior authorizations Correction Requests Complete and submit a Prior Authorization Request Form.Check the Prior Authorization Required List to see if the service requires prior authorization.Please note that authorizations are created per certification period. All services requiring prior authorization must be authorized before providing the service except for services that are necessary on an emergent or truly urgent basis. Unique authorization rules apply for some home health care services. Recertification visit is done during the last five days of the previous certification period.For a re-authorization request (recertification), submit a Narrative Report/Summary of Recertification Visit.For an initial request, submit a Narrative Report/Summary of SOC Visit.To qualify a member for home health care services, you must submit these documents: Required Supporting Clinical Information.


 0 kommentar(er)
0 kommentar(er)
